The number of people suffering from the damaging effects of the disease known as diabetes has exploded decade after decade on a worldwide basis.
According to recent data from the CDC 37.3 million Americans—about 1 in 10—have diabetes. About 1 in 5 people with diabetes don't know they have it. 96 million American adults—more than 1 in 3—have prediabetes. More than 8 in 10 adults with prediabetes don't know they have it. In 2019, about 1.4 million new cases of diabetes were diagnosed.
Chances are, you know someone with diabetes. It may be a friend, a family member, or even you.
The year 2021 marked the 100th anniversary of the discovery of insulin. Before insulin was discovered, people with diabetes didn’t live long lives. The use of insulin has extended diabetics lives but has done nothing to reduce the number of people inflicted with this disease.
People are developing diabetes at younger ages and at higher rates.
If you’re reading this you’re undoubtedly aware that the medical establishment has very little economic interest or incentive to actually get to the root cause of illness, since individuals remaining well doesn’t keep cash flows streaming into bank accounts of medical personnel or stockholders, particularly stockholders of Pharmaceutical companies.
People with diagnosed diabetes have more than twice the average medical costs that people without diabetes have. This is great for the coffers of the medical cartel but devastating economically for individuals suffering with this condition and for anyone paying for health insurance.
The actual cause of the illness known as Diabetes, just like so many other named illnesses, has never really been investigated thoroughly by the medical establishment for the reasons stated above, although there have been some ‘real’ scientists in the past who have tried to reveal the causes.
The link below is to an earlier post that exposes a foundational disease myth held by almost everyone in the the medical industry and perpetrated by medical educational institutions, as well as national public education systems, to the ultimate detriment of every individual on the Earth:
Ending The Virus Myth Is Critical
So just as a SARS-CoV-2 virus does not exist, and is just a group of symptoms, so is diabetes a group of symptoms.
To get a clearer idea of what diabetes really is let’s take a look at some history, by examining some antique medical books.
The first book on diabetes had actually been written in 1798, but its author, John Rollo of England, had only seen three cases of it himself in his twenty-three years of practicing medicine.
The Works of Robert Whytt, a Scottish physician of the early and mid-eighteenth century did not mention diabetes in a 750 page volume.
American physician John Brown, at the end of the eighteenth century, devoted two paragraphs to the disorder in his Elements of Medicine.
In the Works of Thomas Sydenham, who practiced in the seventeenth century and is known as the Father of English Medicine, a single page was focused on diabetes. It set forth a sparse description of the disease, recommended an all-meat diet, and prescribed an herbal remedy.
In Benjamin Ward Richardson’s 500-page work, Diseases of Modern Life, published in New York in 1876, four pages were devoted to diabetes. Richardson considered it a modern disease caused by exhaustion from mental overwork or by some shock to the nervous system. But it was still uncommon.
A book considered a “bible” of diseases of the nineteenth century, the Handbook of Geographical and Historical Pathology, was published in stages between 1881 and 1886 in German and English . In this massive three-volume scholarly work, August Hirsch compiled the history of known diseases, along with their prevalence and distribution throughout the world. Hirsch spared six pages for diabetes, noting primarily that it was rare and that little information about it was known.
In ancient Greece, he wrote, in the fourth century B.C., Hippocrates never mentioned it. In the second century A.D., Galen, a Greek-born physician practicing in Rome, devoted some passages to diabetes, but stated that he himself had seen only two cases.
The statistics Hirsch gathered from around the world confirmed to him that the disease “is one of the rarest.” About 16 people per year died of it in Philadelphia, 3 in Brussels, 30 in Berlin, and 550 in all of England. Occasional cases were reported in Turkey, Egypt, Morocco, Mexico, Ceylon, and certain parts of India. But an informant in St. Petersburg had not seen a case in six years. Practitioners in Senegambia and the Guinea Coast had never seen a case, nor was there any record of it occurring in China, Japan, Australia, the islands of the Pacific, Central America, the West Indies, Guiana, or Peru. One informant had never seen a case of diabetes during a practice of many years in Rio de Janeiro.
How, then, did diabetes come to be one of the major killers of humanity? In today’s world, as we will see, limiting one’s intake of sugar plays an important role in the potential prevention and control of this disease, but does not affect what causes it.
The standard model for diabetes essentially revolves around the consumption of refined sugar overwhelming the ability of the body to maintain metabolic equilibrium.
A typical explanation of this states that we evolved eating foods like potatoes that have to be digested gradually. The pancreas automatically secretes insulin at a rate that exactly corresponds to the rate at which glucose—over a considerable period of time after a meal—enters the bloodstream.
Although this mechanism works perfectly if you eat meat, potatoes, and vegetables, a meal containing refined sugar creates a disturbance. The entire load of sugar enters the bloodstream at once. The pancreas, however, hasn’t learned about refined sugar and responds as though you have just eaten a meal containing a tremendous amount of potatoes. A lot more glucose should be on its way. The pancreas therefore manufactures an amount of insulin that can deal with a tremendous meal. This overreaction by the pancreas drives the blood glucose level too low, starving the brain and muscles—a condition known as hypoglycemia. After years of such overstimulation the pancreas may become exhausted and stop producing enough insulin or produce none at all. This condition is called diabetes and requires the person to take insulin or other drugs to maintain his or her energy balance and stay alive.
It’s notable that an extraordinary rise in sugar consumption has accompanied the equally extraordinary rise in diabetes rates over the past two hundred years.
A century ago Dr. Elliott P. Joslin, founder of Boston’s Joslin Diabetes Center, published statistics showing that yearly sugar consumption per person in the United States had increased eightfold between 1800 in 1917.
So refined sugar and other refined carbohydrates have been given the blame for the dramatic increase of diabetes.
But this model of diabetes is missing an important piece. It teaches us how to potentially avoid getting diabetes in the twenty-first century: don’t eat highly refined foods, especially sugar. But it completely fails to explain the terrible prevalence of diabetes in our time. Sugar or no sugar, diabetes was once an impressively rare disease. The vast majority of human beings were once able to digest and metabolize large quantities of pure sugar without eliminating it in their urine and without wearing out their pancreas.
Even Joslin, whose clinical experience led him to suspect sugar as a cause of diabetes, pointed out that the consumption of sugar in the United States had increased by only 17 percent between 1900 and 1917, a period during which the death rate from diabetes had nearly doubled. And he underestimated sugar use in the nineteenth century because his statistics were for refined sugar only. They did not include maple syrup, honey, sorghum syrup, cane syrup, and especially molasses. Molasses was cheaper than refined sugar, and until about 1850 Americans consumed more molasses than refined sugar.
The following graph shows actual sugar consumption during the past two centuries, including the sugar content of syrups and molasses, and it does not fit the dietary model of this disease. In fact, per capita sugar consumption did not rise at all between 1922 and 1984, yet diabetes rates soared tenfold.
That diet alone is not responsible for the modern pandemic of diabetes is clearly shown by the histories of three communities at opposite ends of the world from one another. One has the highest rates of diabetes in the world today. The second is the largest consumer of sugar in the world. And the third is the most recently electrified country in the world.
American Indians
The poster child for the diabetes story is supposed to be the American Indian. Supposedly—according to the American Diabetes Association—people today are just eating too much food and not getting enough exercise to burn off all the calories. This causes obesity, which, it is believed, is the real cause of most diabetes. Indians, so the story goes, are genetically predisposed to diabetes, and this predisposition has been triggered by the sedentary lifestyle imposed on them when they were confined to reservations, as well as by an unhealthy diet containing large amounts of white flour, fat, and sugar that have replaced traditional foods. And indeed, today, Indians on most reservations in the United States and Canada have rates of diabetes that are the highest in the world.
Yet this does not explain why, since all Indian reservations were created by the end of the nineteenth century, and Indian fry bread, consisting of white flour deep fried in lard and eaten with sugar, became a staple food on most reservations at that time, diabetes nevertheless did not exist among Indians until the latter half of the twentieth century. Before 1940 the Indian Health Service had never listed diabetes as a cause of death for a single Indian.
In 1987, neither diet nor lifestyle in the various communities was different enough to account for a fifty-fold difference in diabetes rates. But one environmental factor could account for the disparities. Electrification came to most Indian reservations later than it came to most American farms. Even in the late twentieth century some reservations were still not electrified. This included most Indian reserves in the Canadian Territories and most native villages in Alaska.
When the first electric service came to the Standing Rock Reservation in the Dakotas in the 1950s, diabetes came to that reservation at the same time.
Brazil
Brazil, which has grown sugar cane since 1516, has been the largest producer and consumer of that commodity since the seventeenth century. Yet in the 1870s, when diabetes was beginning to be noticed as a disease of civilization in the United States, that disease was completely unknown in the sugar capital of the world, Rio de Janeiro.
Brazil today produces over 30 million metric tons of sugar per year and consumes over 130 pounds of white sugar per person, more than the United States. Analyses of the diets of the two countries—Brazil in 2002–2003, and the United States from 1996–2006—revealed that the average Brazilian obtained 16.7 percent of his or her calories from table sugar or sugar added to processed foods, while Americans consumed only 15.7 percent of their calories from refined sugars. Yet the United States had more than two and a half times the rate of diabetes as Brazil.
Bhutan
Sandwiched between the mountainous borders of India and China, the isolated Himalayan kingdom of Bhutan may be the last country in the world to be electrified. Until the 1960s, Bhutan had no banking system, no national currency, and no roads.
As recently as 2002, fuel wood provided virtually one hundred percent of all non-commercial energy consumption. Fuel wood consumption, at 1.22 tons per capita, was one of the highest, if not the highest, in the world. Bhutan was an ideal laboratory in which to monitor the effects of electricity, because that country was about to be transformed from near zero percent electrification to one hundred percent electrification in a little over a decade.
Diabetes was extremely rare, and completely unknown outside the capital.
The Department of Energy and the Bhutan Electricity Authority were created on July 1, 2002. That same day the Bhutan Power Corporation was launched. With 1,193 employees, it immediately became the largest corporation in the kingdom.
Its mandate was to generate and distribute electricity throughout the kingdom, with a target of full electrification of the country within ten years. By 2012 the proportion of rural households actually reached by electricity was about 84 percent.
In 2004, 634 new cases of diabetes were reported in Bhutan. The next year, 944. The year after that, 1,470. The following year, 1,732. The next year, 2,541, with 15 deaths. In 2010, there were 91 deaths and diabetes mellitus was already the eighth most common cause of mortality in the kingdom. Coronary heart disease was number one. Only 66.5 percent of the population had normal blood sugar. This sudden change in the health of the population, especially the rural population, was being blamed, incredibly, on the traditional Bhutanese diet which, however, had not changed.
Only one other thing has changed so dramatically in Bhutan in the last decade: electrification, and the resulting exposure of the population to electromagnetic fields.
By now I’m sure the missing piece of the diabetes model is clear, and that is exposure to electromagnetic fields.
Exposure to electromagnetic fields interferes with basic metabolism. The power plants of our cells, the mitochondria, become less active, slowing the rate at which our cells can burn glucose, fats, and protein. Instead of being taken up by our cells, excess fats accumulate in our blood and are deposited on the walls of our arteries along with the cholesterol that transports them, forming plaques and causing coronary heart disease. This can potentially be prevented by eating a low-fat diet.
In the same way, excess glucose, instead of being taken up by our cells, also backs up and accumulates in our blood. This increases the secretion of insulin by our pancreas. Normally, insulin lowers blood sugar by increasing its uptake by our muscles. But now our muscle cells can’t keep up. They burn glucose as fast as they can after a meal, and it’s no longer fast enough. Most of the excess goes into our fat cells, is converted to fat, and makes us obese.
If your pancreas becomes worn out and stops producing insulin, you have Type 1 diabetes. If your pancreas is producing enough, or too much insulin, but your muscles are unable to use glucose quickly enough, this is interpreted as “insulin resistance” and you have Type 2 diabetes.
Eating a diet free of highly refined, quickly digested foods, especially sugar, can potentially prevent this.
Insulin resistance—which accounts for the vast majority of diabetes in the world today—did not exist before the late nineteenth century. Neither did obese diabetic patients. Almost all people with diabetes were insulin-deficient, and they were universally thin: since insulin is needed in order for muscle and fat cells to absorb glucose, people with little or no insulin will waste away.
They pee away their glucose instead of using it for energy, and survive by burning their stores of body fat.
In fact, overweight diabetics were at first so unusual that late-nineteenth-century doctors couldn’t quite believe the change in the disease—and some of them didn’t.
Today the disease has changed entirely. Even children with Type 1, insulin-deficient diabetes tend to be overweight. They are overweight before they become diabetic because of their cells’ reduced ability to metabolize fats. They are overweight after they become diabetic because the insulin that they take for the rest of their lives makes their fat cells take up lots of glucose and store it as fat.
Diabetes Is Also a Disorder of Fat Metabolism
Nowadays, all blood that is drawn from a patient is sent right off to a laboratory to be analyzed.
The doctor rarely looks at it. But a hundred years ago the quality and consistency of the blood were valuable guides to diagnosis. Doctors knew that diabetes involved an inability to metabolize not just sugar but fat, because blood drawn from a diabetic’s vein was milky, and when it was allowed to stand, a thick layer of “cream” invariably floated to the top. In the early years of the twentieth century, when diabetes had become epidemic and was not yet controllable with any medication, it was not unusual for a diabetic’s blood to contain 15 to 20 percent fat.
Dr. Elliot Joslin even found that blood cholesterol was a more reliable measure of the severity of the disease than blood sugar. He disagreed with those of his contemporaries who were treating diabetes with a low-carbohydrate, high-fat diet. “The importance of the modification of the treatment to include control of the fat of the diet is obvious,” he wrote. He issued a warning, appropriate not only for his contemporaries but for the future: “When fat ceases to be metabolized in a normal manner no striking evidence of it is afforded, and both patient and doctor continue to journey along in innocent oblivion of its existence, and hence fat is often a greater danger to a diabetic than carbohydrate.”
The linked failure of both carbohydrate and fat metabolism is a sign of disordered respiration in the mitochondria, and the mitochondria are disturbed by electromagnetic fields.
Under the influence of such fields, respiratory enzyme activity is slower. After a meal, the cells cannot oxidize the breakdown products of the proteins, fats, and sugars that we eat as quickly as they are being supplied by the blood. Supply outstrips demand. Recent research has shown exactly how this happens.
Glucose and fatty acids, proposed University of Cambridge biochemist Philip J. Randle in 1963, compete with each other for energy production. This mutual competition, he said, operates independently of insulin to regulate glucose levels in the blood. In other words, high fatty acid levels in the blood inhibit glucose metabolism, and vice versa. Evidence in support appeared almost immediately. Jean-Pierre Felber and Alfredo Vannotti at the University of Lausanne gave a glucose tolerance test to five healthy volunteers, and then another one a few days later to the same individuals while they were receiving an intravenous infusion of lipids. Every person responded to the second test as though they were insulin resistant. Although their insulin levels remained the same, they were unable to metabolize the glucose as quickly in the presence of high levels of fatty acids in their blood, competing for the same respiratory enzymes. These experiments were easy to repeat, and overwhelming evidence confirmed the concept of the “glucose-fatty acid cycle.”
Some evidence also supported the idea that not only fats, but amino acids as well, competed with glucose for respiration.
Randle had not been thinking in terms of mitochondria, much less what could happen if an environmental factor restricted the ability of the respiratory enzymes to work at all. But during the last decade and a half, finally some diabetes researchers have begun focusing specifically on mitochondrial function.
Remember that our food contains three main types of nutrients—proteins, fats, and carbohydrates—that are broken down into simpler substances before being absorbed into our blood. Proteins become amino acids. Fats become triglycerides and free fatty acids. Carbohydrates become glucose. Some portion of these is used for growth and repair and becomes part of the structure of our body. The rest is burned by our cells for energy.
Within our cells, inside tiny bodies called mitochondria, amino acids, fatty acids, and glucose are all further transformed into even simpler chemicals that feed into a common cellular laboratory called the Krebs cycle, which breaks them down the rest of the way so that they can combine with the oxygen we breathe to produce carbon dioxide, water, and energy. The last component in this process of combustion, the electron transport chain, receives electrons from the Krebs cycle and delivers them, one at a time, to molecules of oxygen. If the speed of those electrons is modified by external electromagnetic fields, or if the functioning of any of the elements of the electron transport chain is otherwise altered, the final combustion of our food is impaired. Proteins, fats, and carbohydrates begin to compete with each other and back up into the bloodstream. Fats are deposited in arteries. Glucose is excreted in urine. The brain, heart, muscles, and organs become oxygen-deprived. Life slows down and breaks down.
Only recently was it proven that this actually happens in diabetes. For a century, scientists had assumed that because most diabetics were fat, obesity causes diabetes.
But in 1994, David E.Kelley at the University of Pittsburgh School of Medicine, in collaboration with Jean-Aimé Simoneau at Laval University in Quebec, decided to find out exactly why diabetics have such high fatty acid levels in their blood. Seventy-two years after insulin was discovered, Kelley and Simoneau were among the first to measure cellular respiration in detail in this disease. To their surprise, the defect turned out not to be in the cells’ ability to absorb lipids but in their ability to burn them for energy. Large amounts of fatty acids were being absorbed by the muscles and not metabolized. This led to intensive research into all aspects of respiration at the cellular level in diabetes mellitus. Important work continues to be done at the University of Pittsburgh, as well as at the Joslin Diabetes Center, RMIT University in Victoria, Australia, and other research centers.
What has been discovered is that cellular metabolism is reduced at all levels. The enzymes that break down fats and feed them into the Krebs cycle are impaired. The enzymes of the Krebs cycle itself, which receives the breakdown products of fats, sugars, and proteins, are impaired.
The electron transport chain is impaired. The mitochondria are smaller and reduced in number.
Consumption of oxygen by the patient during exercise is reduced. The more severe the insulin resistance—i.e., the more severe the diabetes—the greater the reductions in all these measures of cellular respiratory capacity.
In fact, Clinton Bruce and his colleagues in Australia found that the oxidative capacity of the muscles was a better indicator of insulin resistance than their fat content—which threw into question the traditional wisdom that obesity causes diabetes. Perhaps, they speculated, obesity is not a cause but an effect of the same defect in cellular respiration that causes diabetes. A study involving lean, active young African-American women in Pittsburgh, published in 2014, seemed to confirm this. Although the women were somewhat insulin resistant, they were not yet diabetic, and the medical team could find no other physiological abnormalities in the group except two: their oxygen consumption during exercise was reduced, and mitochondrial respiration in their muscle cells was reduced.
In 2009, the Pittsburgh team made an extraordinary finding. If the electrons in the electron transport chain are being disturbed by an environmental factor, then one would expect that diet and exercise might improve all components of metabolism except the last, energy-producing step involving oxygen. That is exactly what the Pittsburgh team found. Placing diabetic patients on calorie restriction and a strict exercise regime was beneficial in many respects. It increased the activity of the Krebs cycle enzymes. It reduced the fat content of muscle cells. It increased the number of mitochondria in the cells. These benefits improved insulin sensitivity and helped control blood sugar. But although the number of mitochondria increased, their efficiency did not. The electron transport enzymes in dieted, exercised diabetic patients were still only half as active as the same enzymes in healthy individuals.
In June 2010, Mary-Elizabeth Patti, a professor at Harvard Medical School and researcher at the Joslin Diabetes Center, and Silvia Corvera, a professor at the University of Massachusetts Medical School in Worcester, published a comprehensive review of existing research on the role of mitochondria in diabetes. They were forced to conclude that a defect of cellular respiration may be the basic problem behind the modern epidemic. Due to “failure of mitochondria to adapt to higher cellular oxidative demands,” they wrote, “a vicious cycle of insulin resistance and impaired insulin secretion can be initiated.”
But they were not willing to take the next step. No diabetes researchers today are looking for an environmental cause of this “failure to adapt” of so many people’s mitochondria. They are still, in the face of evidence refuting it, blaming this disease on faulty diet, lack of exercise, and genetics. This in spite of the fact that, as Dan Hurley noted in his 2011 book, Diabetes Rising, human genetics has not changed and neither diet, exercise, nor drugs has put a dent in the escalation of this disease during the ninety years since insulin was discovered.
Diabetes in Radio Wave Sickness
In 1917, when Joslin was publishing the second edition of his book on diabetes, radio waves were being massively deployed on and off the battlefield in the service of war. At that point radio waves joined power distribution as a leading source of electromagnetic pollution on this planet. Their contribution has steadily grown until today when radio, television, radar, computers, cell phones, satellites, and millions of transmission towers have made radio waves by far the predominant source of electromagnetic fields bathing living cells.
The effects of radio waves on blood sugar are extremely well documented. However, none of this research has been done in the United States or Europe. It has been possible for western medical authorities to pretend that it doesn’t exist because most of it is published in Czech, Polish, Russian, and other Slavic languages in strange alphabets and has not been translated into familiar tongues.
But some of it has, thanks to the United States military, in documents that have not been widely circulated, and thanks to a few international conferences.
During the Cold War, from the late 1950s through the 1980s, the United States Army, Navy, and Air Force were developing and building enormously powerful early warning radar stations to protect against the possibility of nuclear attack. In order to stand sentinel over the air spaces surrounding the United States, these stations were going to monitor the entire coastline and the borders with Mexico and Canada. This meant that a strip of the American border up to hundreds of miles wide—and everyone who lived there—was going to be continuously bombarded with radio waves at power levels that were unprecedented in human history. Military authorities needed to review all ongoing research into the health effects of such radiation. In essence, they wanted to know what were the maximum levels of radiation to which they could get away with exposing the American population. And so one of the functions of the Joint Publications Research Service, a federal agency established during the Cold War to translate foreign documents, was to translate into English some of the Soviet and Eastern European research on radio wave sickness.
One of the most consistent laboratory findings in this body of literature is a disturbance of carbohydrate metabolism.
In the late 1950s, in Moscow, Maria Sadchikova gave glucose tolerance tests to 57 workers exposed to UHF radiation. The majority had altered sugar curves: their blood sugar remained abnormally high for over two hours after an oral dose of glucose. And a second dose, given after one hour, caused a second spike in some patients, indicating a deficiency of insulin.
In 1964, V. Bartoníček, in Czechoslovakia, gave glucose tolerance tests to 27 workers exposed to centimeter waves—the type of waves we are all heavily exposed to today from cordless phones, cell phones, and wireless computers. Fourteen of the workers were prediabetic and four had sugar in their urine. This work was summarized by Christopher Dodge in a report he prepared at the United States Naval Observatory and read at a symposium held in Richmond, Virginia in 1969.
In 1973, Sadchikova attended a symposium in Warsaw on the Biologic Effects and Health Hazards of Microwave Radiation. She was able to report on her research team’s observations of 1,180 workers exposed to radio waves over a twenty-year period, of whom about 150 had been diagnosed with radio wave sickness. Both prediabetic and diabetic sugar curves, she said, “accompanied all clinical forms of this disease.”
Eliska Klimková-Deutschová of Czechoslovakia, at the same symposium, reported finding an elevated fasting blood sugar in fully three-quarters of all individuals exposed to centimeter waves.
Valentina Nikitina, who was involved in some of the Soviet research and was continuing to do such research in modern Russia, attended an international conference in St. Petersburg in 2000. She reported that people who maintained and tested radio communication equipment for the Russian Navy—even people who had ceased such employment five to ten years previously—had, on average, higher blood glucose levels than unexposed individuals.
Attached to the same medical centers at which Soviet doctors were examining patients were laboratories where scientists were exposing animals to the very same types of radio waves. They, too, reported seriously disturbed carbohydrate metabolism. They found that the activity of the enzymes in the electron transport chain, including the last enzyme, cytochrome oxidase, is always inhibited. This interferes with the oxidation of sugars, fats and proteins. To compensate, anaerobic (non-oxygen using) metabolism increases, lactic acid builds up in the tissues, and the liver becomes depleted of its energy-rich stores of glycogen. Oxygen consumption declines. The blood sugar curve is affected, and the fasting glucose level rises. The organism craves carbohydrates, and the cells become oxygen starved. These changes happen rapidly.
As early as 1962, V. A. Syngayevskaya, working in Leningrad, exposed rabbits to low level radio waves and found that the animals’ blood sugar rose by one-third in less than an hour. In 1982, Vasily Belokrinitskiy, working in Kiev, reported that the amount of sugar in the urine was in direct proportion to the dose of radiation and the number of times the animal was exposed. Mikhail Navakatikian and Lyudmila Tomashevskaya reported in 1994 that insulin levels decreased by 15 percent in rats exposed for just half an hour, and by 50 percent in rats exposed for twelve hours, to pulsed radiation at a power level of 100 microwatts per square centimeter. This level of exposure is comparable to the radiation a person receives today sitting directly in front of a wireless computer, and considerably less than what a person’s brain receives from a cell phone.
If there wasn’t a public outcry when most of this information was concealed in foreign alphabets, there should be one now, because it has become possible to confirm directly, in human beings, the degree to which cell phones interfere with glucose metabolism, and the outcomes of such studies are being published in English.
Finnish researchers reported their alarming findings in the Journal of Cerebral Blood Flow and Metabolism in 2011. Using positron emission tomography (PET) to scan the brain, they found that glucose uptake is considerably reduced in the region of the brain next to a cell phone.
Even more recently, researchers at Kaiser Permanente in Oakland, California, confirmed that electromagnetic fields cause obesity in children. They gave pregnant women meters to wear for 24 hours to measure their exposure to magnetic fields during an average day. The children of those women were more than six times as likely to be obese when they were teenagers if their mothers’ average exposure during pregnancy had exceeded 2.5 milligauss. Of course, the children were exposed to the same high fields while growing up, so what the study really proved is that magnetic fields cause obesity in chidren.
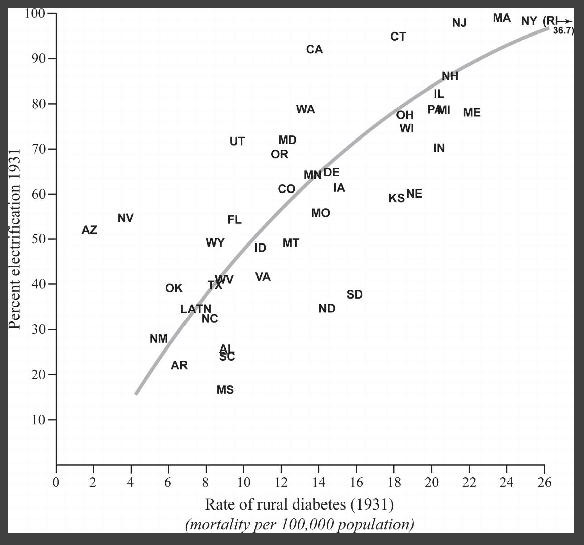
Rural mortality from diabetes in the 1930’s corresponded closely with rates of rural electrification, and varied as much as tenfold between the least and the most electrified states.
The following chart shows the direct correlation:
Mortality from diabetes increased steadily from 1870 until the 1940s—this, despite the discovery of insulin in 1922.
The apparent drop in mortality in 1950 is not real, but is due to a reclassification that occurred in 1949. Previously, if a person had both diabetes and heart disease, the cause of death was reported as diabetes. Beginning in 1949, those deaths were reported as due to heart disease, diminishing the reported mortality from diabetes by about 40 percent. In the late 1950s, Orinase, Diabinase, and Phenformin were brought to market, the first of many oral medications that helped control the blood sugar of people with “insulin-resistant” diabetes for whom insulin was of limited use. These drugs have restrained, but not reduced the mortality from this disease.
Meanwhile the number of diagnosed cases of diabetes in the United States has steadily increased.
The real change over time may have been even greater because the definition of diabetes, in the United States and worldwide, was relaxed in 1980. A two-hour plasma glucose level of over 130 milligrams per deciliter was formerly taken as an indication of diabetes, but since 1980 diabetes is not diagnosed until the two-hour level exceeds 200 milligrams per deciliter. Levels between 140 and 200, which may not cause sugar in the urine, are now called “prediabetes.”
A sudden spike in diabetes cases occurred nationwide in 1997—a 31 percent increase in a single year. No one was able to explain why. But that was the year the telecommunications industry introduced digital cell phones en masse to the United States. The first such phones went on sale in dozens of American cities during the Christmas season of 1996. Construction of cell towers began in those cities during 1996, but 1997 was the year that battalions of towers, previously confined to metropolises, marched out over the rural landscapes to occupy previously virgin territory. That was the year cell phones were transformed from a rich person’s luxury to the common person’s soon-to-be necessity—the year microwave radiation from towers and antennas became inescapable over large parts of the United States.
Worldwide, it was estimated that more than 180,000,000 adults had diabetes in 2000. In 2014, the estimate was 387,000,000. In no country on earth is the rate of diabetes, or of obesity, decreasing.
This deliberate world wide deadly radiation exposure of humanity is just one more method of parasitism and genocide perpetrated by millions of individuals who are willing to turn their backs on those who are damaged and ultimately murdered.







No offense taken. There's still a lot we don't know about how EMF affects the body, since most 'scientists' and their funding organizations aren't interested in considering health damaging effects, although there are thousands of studies discussing some of these health issues.
When it comes to standard models in the biological 'sciences' and the Medical Industry in general, I've always been skeptical, but my level of skepticism has risen dramatically since I became aware that the murderous plandemic we're continuing to suffer through was based on a non-existent virus. Viruses don't even exist. This is a monumental lie that has resulted and will continue to result in countless numbers of deaths.
This is been a problem for me. I know I’m not type two diabetic. I am EMF hypersensitive, so one day I’m normal if my EMF exposure is small, but if it’s too high, then I look like I’m diabetic. I have to take a walk for an hour just to lower my blood sugar before I do any type of medical physical for my job.